Treatment of AV Fistula and Graft Malfunction
What is the endovascular treatment of AV fistula graft malfunction?
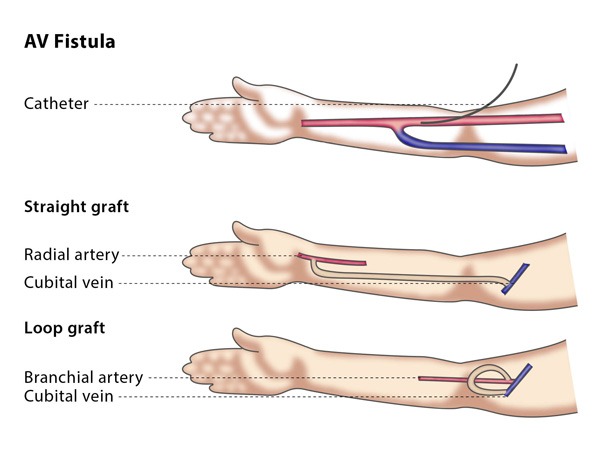
An AV fistula is an abnormal connection between an artery and a vein, and is sometimes surgically created to help with haemodialysis treatment. In these cases, a shunt graft is inserted to aid the treatment.
Unfortunately, sometimes the shunt will fail, known as graft malfunction. If you experience this, your doctor may recommend that you have endovascular treatment. The aim of this minimally invasive procedure is to stop narrowing of the fistula and remove any blockages from the shunt, such as blood clots.
The techniques used in the procedure depend on the type of lesion as well as its location.
How does the procedure work?
The interventional radiologist will usually enter the AV fistula through a direct puncture into the shunt, though they may instead choose to enter through a puncture in your elbow flexure or in your groin. The interventional radiologist will choose the entry point and technique depending on the condition which needs to be treated (such as narrowing of the fistula or a blood clot in the shunt) and its location.
If you have a narrowing of the AV fistula, the interventional radiologist may perform a technique called percutaneous transluminal angioplasty (PTA), which involves inserting and expanding a balloon to widen the vessel.
In rare cases, such as if the AV fistula starts to narrow again (restenosis) or if the area has been injured during the procedure, the interventional radiologist may insert a metal mesh tube (a stent) into the fistula. This acts like a skeleton and keeps the vessel open by supporting the walls of the vein. You may also need to take medication to prevent blood clots forming, but this depends on the PTA, the stent and your clinical situation.
If you have a blood clot, it can be sucked out by a vacuum, or mechanical devices can be used to break it up. These devices are applied over the sheath into the thrombus.
These techniques may need to be followed by catheter thrombolysis, in which medication is inserted through a catheter to break up the thrombus. If you undergo combined therapy with a thrombectomy or thrombolysis, you will be kept under observation for 24-48 hours with repeated follow-ups using angiography.
Why perform it?
The endovascular treatment of AV fistula graft malfunction is recommended to prevent or reverse blockages and so restore the function of the AV fistula and shunt.
There are a number of techniques and tools which your interventional radiologist may use, depending on the problem. If you have a stenosis (narrowing), the best treatment option is a balloon which can be inserted and gently inflated, while if you have a blood clot, a combination of thrombectomy, thrombolysis and medication to prevent blood clotting may be recommended.
What are the risks?
Minor risks include bruising at the puncture site in your neck or groin or in the affected limb. Major risks include injury to the wall of the blood vessel, which can happen if the devices are used incorrectly. You may experience bleeding if you undergo thrombolysis.
Bibliography
1. Beathard GA. Mechanical versus pharmacomechanical thrombolysis for the treatment of thrombosed dialysis access grafts. Kidney international. 1994; 45(5):1401-6.
2. Glanz S, Gordon DH, Butt KM, Hong J, Lipkowitz GS. The role of percutaneous angioplasty in the management of chronic hemodialysis fistulas. Annals of surgery. 1987; 206(6):777-81.
3. Gmelin E, Karnel F. Radiologic recanalization of veins, vascular prostheses and arteries in cases of insufficient dialysis fistulas. RoFo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 1990; 153(4):432-7. Radiologische Rekanalisation von Venen, Gefassprothesen und Arterien bei insuffizienten Dialysefisteln.
4. Keller E, Reetze-Bonorden P, Lucking HP, Bohler J, Schollmeyer P. Continuous arteriovenous hemodialysis: experience in twenty-six intensive care patients. Contributions to nephrology. 1991; 93:47-50.
5. Vorwerk D. Non-traumatic vascular emergencies: management of occluded hemodialysis shunts and venous access. European radiology. 2002; 12(11):2644-50.
